Abstract

Background:
Donor erythrocyte (RBC) transfusion was the first therapy used in sickle cell disease (SCD) that targets the pathophysiology of sickle cell disease.1 Transfused RBCs represent iron that circumvents the normal pathways of iron regulation, this excess iron accumulates in tissues.2 Iron overload was present in one third of 141 adult SCD patients at post mortem (mean age, 36 years) and 7% of deaths were related to iron overload.3 In a cohort of 387 young adults from Atlanta, there were 22 deaths, 45% related to iron overload (cirrhosis: 9, heart failure: 2).4 The frequency of hospital admission increased with increased serum ferritin in 199 transfused SCD patients, although the extent to which iron overload was a cause or a consequence of disease severity was not clear.5 We designed a study to retrospectively review the clinical course of SCD patients with iron overload compared to those without iron overload.
Methods:
We retrospectively reviewed 105 patients at the sickle cell comprehensive clinic at the study institution from Jan 1, 1998 to Oct 31, 2016. Patients with Hb SS, HSC and HB S beta0thalassemia were included. Iron overload was defined as mean serum ferritin >1000 ng/ml and/or T2 liver MRI with hepatic iron content >3 mg/g dry weight. Clinical outcomes studied as categorical variables were liver disease - defined as hepatomegaly, coagulopathy, signs of portal HTN or cirrhosis, thyroid disease - symptoms or abnormal thyroid functions, hypogonadism - history or laboratory measurement of gonadotrophins, arthropathy - symptoms or radiological evidence of joint disease and congestive heart failure - symptoms or low left ventricular ejection fraction on echocardiogram. Clinical outcomes that were studied as continuous variables were number of hospitalization during study period and mean body mass index. Patients who were on chelation at any time were analyzed separately as a subgroup within the iron overload cohort. The categorical variables were analyzed by using Chi-Square test and numerical variable was analyzed using t-test for equality of means.
Results:
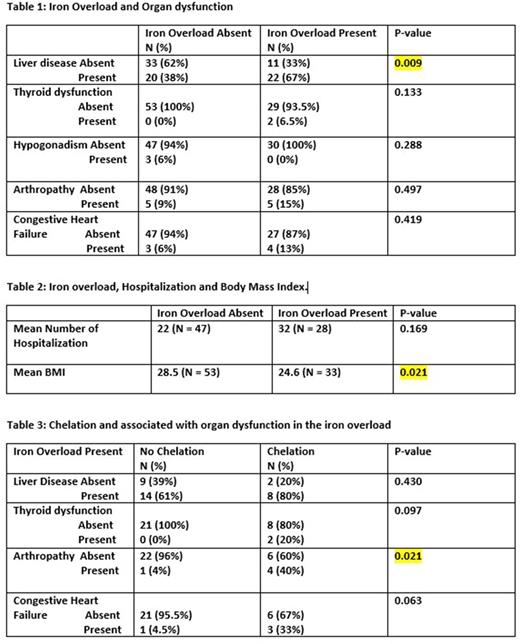
86 out of 105 patients had complete data for clinical outcomes. Out of 33 patients with iron overload 22 had liver disease (66.7%) as compared to only 20 out of 53 (37.7%) without iron overload (p-value =0.009 which was significant). Out of 31 patients with iron overload only 2 (6.5%) had thyroid disease as compared to 0 out of 53 patients (0%) without iron overload. Out of 30 patients with iron overload 0 (0%) had hypogonadism as compared to 3 out of 50 patients (6%) without iron overload. 5 out of 33 patients with iron overload (15.2%) had arthropathy as compared to 5 out of 53 without iron overload (9.4%). 4 out of 31 patients with iron overload had congestive heart failure (12.9%) compared to 3 out of 50 patients without iron overload (6.0%).
A total of 10 out of 33 patients (30.3%) with iron overload got chelation at some time during the study period. 8 out of 10 patients (80%) with iron overload who got chelation had liver disease compared to 14 out of 23 patients (60%) with iron overload and no chelation. 2 out 10 patients (20%) who got chelation had thyroid disease compared to 0 out of 21 (0%) without chelation. Interestingly, 4 out of 10 patients (40%) who got chelation had arthropathy compared to 1 out of 23 (4.3%) without chelation (p-value = 0.021 which was significant). 3 out of 9 patients (33.3%) who got chelation had congestive heart failure compared to 1 out of 22 patients (4.5%) without chelation.
The mean number of hospitalizations in the iron overload group was 32.07 vs 21.74 in the non-iron overload group during the study period (p-value = 0.169). The mean BMI was 24.59 in the iron overload group compared to 28.48 in the non-iron overload group (p-value = 0.021 was significant).
Conclusion:
Iron overload was associated with significantly more incidence of liver disease in SCD patients. Chelation was not associated with a statistical significant difference on the incidence of liver disease in the iron overload cohort. There was no significant differences observed in congestive heart failure, hypogonadism or arthropathy. However, patients who were chelated did have a significantly higher incidence of arthropathy. There was no statistically significant difference in the number of hospitalization. Patients with iron overload did have a statistical significant association with having lower BMI.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal